Claudication
Claudication ("limping" in Latin) is pain, aching, or fatigue in muscles of the buttocks, thigh, or calf that occurs with exertion and resolves with rest. Claudication is caused by atherosclerosis (poor circulation) of the blood to the lower extremities, a condition commonly known as Peripheral Artery Disease (PAD).
Claudication, if left untreated, can progress to critical limb ischemia--a severe obstruction of blood flow to the extremities--often accompanied by severe pain and/or skin ulcers or sores with the risk of amputation. UCSF Vascular Surgeons and their multidisciplinary team will do a careful assessment of each patient and develop a personalized treatment plan based on the severity of the condition and the best likelihood of a successful outcome.
Atherosclerosis is the hardening and narrowing of the arteries over time thorough a build-up of plaque. Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows the arteries blocking the flow of blood through them. This limits the flow of oxygen-rich blood to organs and other parts of of the body.
Twelve percent of the U.S. population, or nine million people, experience occasional claudication, with twenty percent of those people over 70. Individuals with intermittent claudication may also have diabetes—often undiagnosed.
Development and Progression
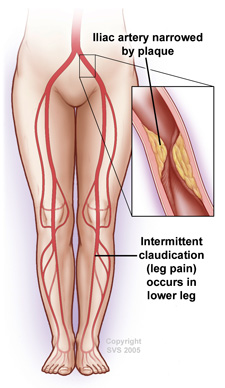 In the early stages of PAD, patients may experience cramping or fatigue in the legs or buttocks while walking or exercising. This is referred to as "intermittent claudication." Claudication may occur in one or both legs, depending on where the blockage is. The pain, or other symptoms subside when the activity is stopped. Claudication pain can range from mild to disabling.
In the early stages of PAD, patients may experience cramping or fatigue in the legs or buttocks while walking or exercising. This is referred to as "intermittent claudication." Claudication may occur in one or both legs, depending on where the blockage is. The pain, or other symptoms subside when the activity is stopped. Claudication pain can range from mild to disabling.
Claudication, if left untreated, can progress to critical limb ischemia, a severe obstruction of blood flow to the extremities, often accompanied by severe pain and/or skin ulcers or sores.
Symptoms
- Pain in the buttocks, thigh, or calf while walking that resolves at rest
- Tired or burning sensation in the buttocks, thigh or calf while walking or exercising
Risk Factors
Risk factors for claudication are the same as those for atherosclerosis:
- Age
- Smoking
- Diabetes
- Being overweight or obese
- Sedentary lifestyle
- High cholesterol
- High blood pressure (hypertension)
- Family history of atherosclerosis or claudication
Diagnosis
- Auscultation - The presence of a bruit (“whooshing” sound), in the arteries of the legs, confirmed using a stethoscope.
- Ankle-brachial index (ABI) - Systolic blood pressure in the ankle divided by the systolic pressure at the arm.
- Doppler Ultrasound - A type of ultrasound that can measure the direction and velocity of blood flow through the vessels.
- CT Angiography - An advanced X-ray procedure using a computer to generate three-dimensional images of blood vessels.
- Magnetic Resonance Angiography (MR angiography) - Patient is exposed to radiofrequency waves in a strong magnetic field. The energy released is measured and utlized to create two- and three-dimensional images of the blood vessels.
- Angiogram - An X-ray study of the blood vessels using contrast dyes.
Lifestyle Changes and Medical Therapy
These include:
- Smoking cessation
- Walking, usually 30 minutes a day
- Medication and lifestyle changes aimed at reducing cholesterol, blood pressure and blood-sugar levels
- Medication, such as aspirin, to prevent heart attack and stroke
- Medication to improve walking distance, such as cilostazol (Pletal)
- Diet low in saturated fats
- Exercise and weight loss
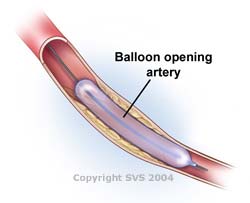
Endovascular Procedures
For patients with severe PAD, attempts to improve blood flow in the leg are usually indicated. The goals of improving blood flow to the limb are to reduce pain, improve functional ability and quality of life, and to prevent amputation.
- The overall health of the patient.
- History of their vascular problem and prior treatments.
- Location and severity of the arterial blockages in the leg.
 |
 |
|
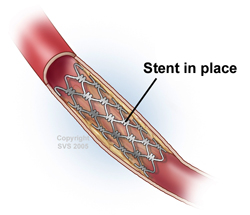
| Angioplasty - A tiny balloon is inserted through a puncture in the groin. The balloon is inflated using a saline solution to expand the narrowed (occluded) artery. | Stenting - Metal mesh tubes are expanded and left in place to provide scaffolding for an artery that has been opened using a balloon angioplasty. |
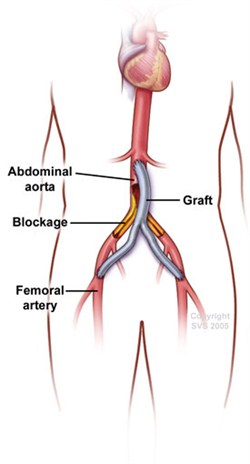
Lower Extremity Bypass Surgery
For patients who are not good candidates for angioplasty, or who have already failed a prior angioplasty attempt, lower extremity bypass surgery is a well-established and highly effective procedure.
In these procedures, surgeons create an alternative conduit for blood flow to circumvent the area of blockage and restore direct flow to the lower leg and foot. This is a major surgical procedure performed under anesthesia via incisions in the leg.
Careful assessment of the risks and benefits prior to surgery, as well as diligent medical, anesthetic, and surgical care, insures the best outcomes following leg bypass operations.
For more information see Lower Extremity Bypass Surgery