Chronic Venous Insufficiency
UCSF vascular surgeons have extensive experience with the latest minimally invasive approaches for treatment of venous disease including radiofrequency (RF) vein ablation, a technique in which a catheter delivers microwave radiation to seal veins that have reflux. This promotes faster healing and a return to work in days instead of weeks.
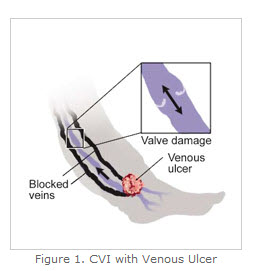 Chronic venous insufficiency (CVI) describes a condition affecting the veins in the lower extremities (legs) with venous hypertension. This leads to pain, swelling, edema, skin changes, and ulcerations in the legs.
Chronic venous insufficiency (CVI) describes a condition affecting the veins in the lower extremities (legs) with venous hypertension. This leads to pain, swelling, edema, skin changes, and ulcerations in the legs.
Chronic venous insufficiency is also called "venous reflux". Venous reflux occurs when venous valves don't function adequately, leading to reversal of blood flow through the valves during standing or sitting. Venous reflux most commonly occurs when vein valves weaken due to genetic influences or multiple pregnancies, among other factors.
When the valves in the veins of the lower body do not properly channel blood flow back to the heart because of blockage or venous valve malfunction, blood flow slows, pressure increases, and swelling occurs in the legs and feet. Venous reflux is often self-perpetuating, as the pooling of blood in veins distends them, which pulls apart the valve leaflets of the next, lower valve and causes reflux farther down the leg.
As blood pools in lower extremities, veins further swell, leading to pain, pigmentation of the skin, and clots in the varicose veins (phlebitis).
Causes
CVI is caused by long-term blood pressure that is higher than normal inside the leg veins. Phlebitis and deep vein thrombosis might lead to CVI.
Factors that can increase the risk of CVI include:
- Family history of varicose veins
- Being overweight
- Being pregnant
- Not enough exercise
- Smoking
- Standing or sitting for long periods of time
- Women over 50 years old have a higher risk of developing CVI
Signs and Symptoms
The symptoms of chronic venous insufficiency are:
- Persistent swelling of the lower legs
- Leg pain, dull aching, heaviness or cramping.
- Bluish discoloration of the skin at the ankles.
- With prolonged swelling, venous ulcers can develop at the ankles and these often become infected
Diagnosis
The following diagnostic procedures may be used to diagnose chronic venous insufficiency:
Duplex Ultrasound - A vascular ultrasound procedure performed to assess blood flow and the structure of the leg veins. The term "duplex" refers to two modes of ultrasound: Doppler and B-mode. The B-mode transducer (like a microphone) obtains an image of the blood vessel of interest. The Doppler probe within the transducer measures the velocity and direction of blood flow within the vessel.
Magnetic Resonance Venography (MRV) - A diagnostic procedure utilizing a combination of a large magnet, radio frequencies, and a computer to produce detailed images of bodily organs and structures. An MRV uses magnetic resonance technology and intravenous (IV) contrast dye to visualize the veins. Contrast dye causes the blood vessels to appear opaque on the x-ray, enabling the physician to visualize the blood vessels being studied. MRV can also help detect causes of leg pain other than vein problems.
Treatments
Chronic Venous Insufficiency
The goals of treatment are to reduce swelling and improve the return of blood to the heart.
- Elevating the legs above the heart (when not standing) helps to return blood to the heart, decrease blood pooling, and decrease swelling.
- Exercise that stimulates calf muscles and increases circulation.
Venous Ulcers
Venous ulcers are open sores in the skin that occur with sustained venous hypertension and malfunctioning of venous valves. Ulcers develop in areas where blood collects and pools, as swelling there interferes with the movement of oxygen and nutrients through the tissues. Eventually, a visible ulcer develops on the skin. Venous ulcers usually occur just above the ankle on the inside of the leg.
If left untreated, venous ulcers can quickly become infected, leading to cellulitis or gangrene and the risk of foot or leg amputation.
Treatments for venous ulcers include:
- Compression Stockings - The most common treatment for venous insufficiency is compression stockings which apply constant, even pressure to the leg. This increases circulation and prevents blood from flowing backward, thereby reducing swelling. Compression stockings can also help prevent venous ulcers from forming, or can help to speed the healing of an existing ulcer. Compression stockings must be worn daily to be effective. Doctors may also prescribe blood thinners, especially in patients with a high risk of blood clots.
- Unna Boots - An Unna boot is a moist gauze bandage applied around the lower leg starting at the area of the ulcer to just below the knee. The gauze hardens to form a snug boot on the leg. The support from the boot improves blood flow in the veins and aids in the healing of the ulcer. The boot is left on for up to two weeks and is replaced if the wound has not healed.
- Transparent Dressings - These are clear plastic-like films that are applied over the wound. The dressing is changed every five to seven days. A support stocking is worn over the dressing to hold the dressing in place and improve circulation in the leg and foot.
- Hydrocolloid Dressings - A hydrocolloid dressing is a special bandage with a breathable outer layer to keep liquid, bacteria, and viruses out, and an inner layer to absorb drainage from the wound and promote healing. The dressing also functions as a debridement therapy to remove any dead or non-viable tissue.
Surgical Therapies
Surgery may be performed for chronic venous insufficiency that fails to respond to other therapies, or for non-healing or infected venous ulcers. Either an open procedure or a catheter-based interventional treatment may be used.
Debridement - Debridement is often done when a venous ulcer shows signs of infection such as when there is fever, elevated white blood count, and persistent or increased drainage. Debridement involves removing infected tissue and bone, nonviable (necrotic or dead) tissue, foreign debris, and residual material from dressings. This process activates the production of platelets, a blood component, and growth factors, both of which promote healing.
Minimally Invasive Therapies
Radiofrequency (RF) Vein Ablation - UCSF vascular surgeons offer the most advanced treatments for venous disorders, including minimally invasive approaches, such as radiofrequency (RF) vein ablation, a technique in which a catheter uses microwave radiation to seal veins that have reflux. Radiofrequency ablation allows doctors to eliminate venous reflux with a needle puncture that is covered with a band-aid versus traditional procedures that require two painful incisions. Patients undergoing RF ablation are able to return to work in days instead of weeks.